Cut Denials. Get Paid Faster.
Automate Revenue Recovery with the RCM AI Agent Built for Specialty Clinics
Most clinics lose 18%+ of their revenue to billing failures. Our AI flags pre-auth gaps, denial risks, and coding errors—before you submit.

If You Are a Clinic Experiencing...
High denial rates and delays
The agent flags pre-auth and coding issues before submission—no surprises at adjudication.
Undercoded procedures cutting your reimbursement
CPT/ICD-10 checker ensures correct reimbursement on high-value procedures.
Claims stuck in your RCM
Agent alerts admins when claims are left in draft or error status.
Preauth and Appeals taking weeks to resolve
The agent drafts, routes, and flags appeal responses instantly—no more 30-day delays or missed opportunities.
Claims stuck in draft or error status
The agent monitors all claims and alerts admins when submissions are stalled or incomplete.
No insight into denial patterns
Denials are tracked, categorized, and surfaced in trend dashboards—so you can fix root causes proactively.
Three steps to cleaner claims and faster cash flow.
Connect
Understand
Resolve
Core Features
Pre-Authorization Detection
Denial Management AI
Code Validator
Claim Submission Readiness
A/R Performance Tracker
Specialty Tuning
Benefits
Get Paid What You're Owed—Faster
- Reduces claim denials and submission errors
- Improves cash flow predictability for reinvestment and growth
- Shortens the collections cycle from 60+ days to as few as 12
Remove 80% of the Admin Grind
- Automatically detects missing pre-auths, code mismatches, and payer rule violations
- Eliminates repetitive denial handling and manual follow-ups
- Transforms your billing team into a strategic, insight-driven function
Capture Revenue That Was Leaking Through the Cracks
- Identifies and alerts for claims left in draft or error status
- Ensures no claim is forgotten or stalled
- Surfaces recurring issues, payer trends, and process gaps before they cost you
Built for Your Specialty
- Preloaded with specialty-specific CPT/ICD-10 logic for high-complexity domains like neurosurgery, orthopedics, and cardiology
- Handles advanced scenarios like bundling, implants, and surgical modifiers
- Co-developed with RCM consultants to ensure relevance and compliance
Common Problems & AI Solutions
Problem
Manual RCM Reality
With RCM AI Agent
Case Studies
BitLab specializes in helping medical professionals convert medical insights into compliant, investor-ready healthtech platforms.
Deep EMR/EHR/PMS Integration Expertise


















and 40+ others
Technologies and Platforms We Use
Neurosurgery Clinic – Lost $7K on a Single Case Due to a Missed Pre-Auth
A busy neurosurgery clinic was preparing a patient for a $75,000 spinal fusion procedure. The front desk scheduled the patient, but missed a critical pre-authorization step because the requirement varied by payer and procedure complexity.
The claim was submitted but got denied due to a missing pre-auth. The clinic scrambled to resubmit with supporting documentation, which added 14 days of delay. When reimbursed, the claim was undercoded, and the practice was only paid $60,000. After a 30-day appeal process, they recovered $68,000—still short.
- $7,000 lost revenue
- 44 days delay
- $800 in staff time wasted chasing appeals
The AI would have:
- Detected the payer’s pre-auth requirement at scheduling
- Auto-prepared and submitted documentation before the appointment
- Flagged coding inconsistencies before the first submission
→ Full reimbursement
→ Zero appeal backlog
→ Staff hours reallocated to high-value tasks

Multi-Specialty Clinic – Denials Were the Norm, Not the Exception
A 10-provider clinic processing 800+ claims/month was seeing a 15% denial rate, mostly from minor errors: mismatched ICD-10/CPT codes, unchecked modifiers, and missing NPI fields. Staff were stuck in a denial loop: resubmit, wait, repeat.
- Claims denied for trivial issues
- Appeals backlog growing
- Delayed cash flow affecting payroll
- Staff burnout rising
- ~$20,000/month in delayed collections
- Denial resubmission turnaround averaged 21 days
- 30+ hours/month spent manually correcting rejections
- Each claim is auto-validated for payer-specific formatting
- CPT/ICD-10 pairings are double-checked
- Missing fields flagged before submission
- Denial reasons are parsed and appeals suggested in real time
→ Denial rate dropped from 15% to 6%
→ $16,000+/month recovered
→ 50% fewer hours spent on resubmissions

Orthopedic Group – Claims Were “Stuck” in the PMS and No One Knew
An orthopedic group’s billing team was surprised to find over 180 claims were never submitted—they were sitting in a "draft" status in their PMS due to system quirks and human oversight. These claims had been sitting idle for weeks.
- $110,000 in claims were never sent to payers
- The PMS offered no real-time alerts
- Aging AR ballooned without anyone noticing
- Thousands in lost or delayed revenue
- Operational chaos trying to retroactively fix the backlog
- Missed payment windows on several claims
- The agent continuously monitored claim statuses
- Triggered alerts for any claims idle >48 hours
- Escalated high-value drafts to billing leads for review
→ 100% of claims submitted within 72 hours
→ Prevented $100K+ in leakage over 3 months
→ Created a proactive, not reactive, billing team culture

Why It Works
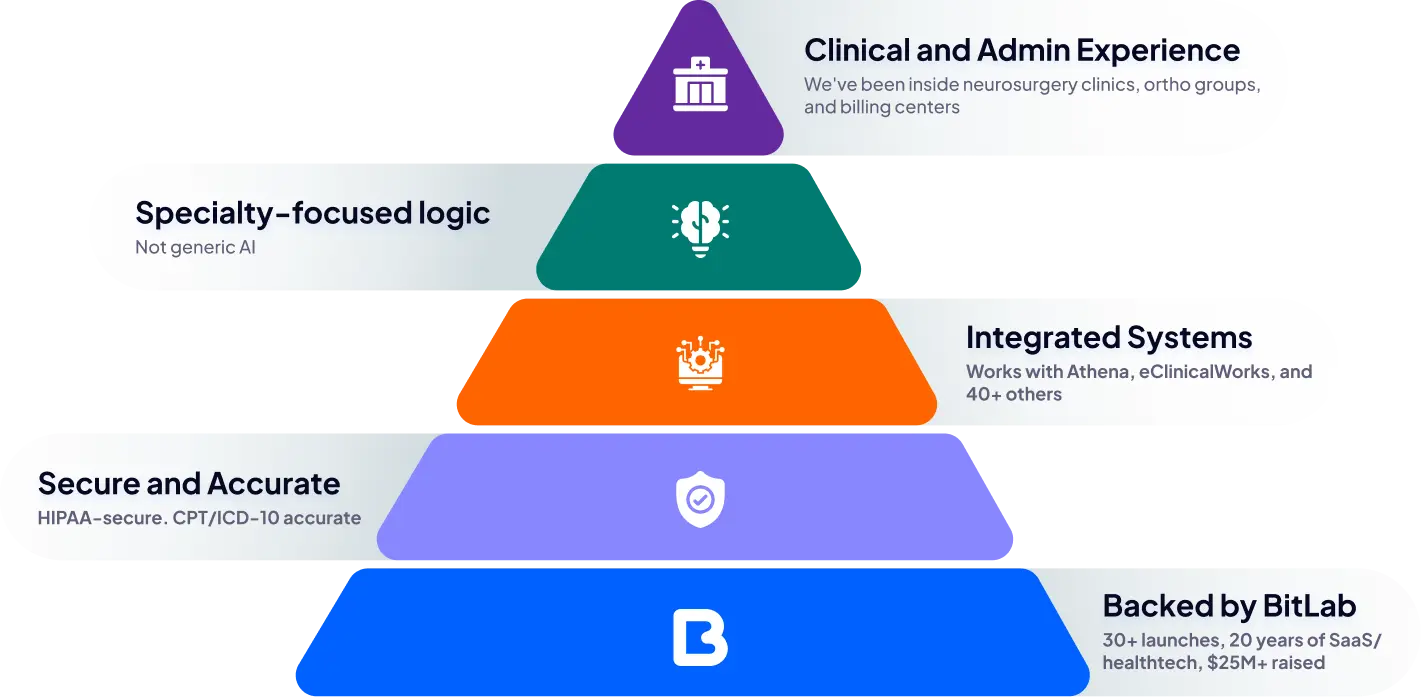
Built with experts from…











Deep EMR/EHR/PMS Integration Expertise

Protecting Our Patients' Information

Robust Security

Data Privacy

PIPEDA and Regional Compliance
- Provincial regulations like PHIPA, PIPA, HIA, PHIA, and PHIPAA.
- Specific compliance for Quebec’s TGV (Travailleur Général Virtuel) standards.
Don’t just take our word for it
Your Questions, Answered
Our minimum budget on projects starts at $30,000. This ensures we can dedicate the necessary resources to deliver high-quality solutions tailored to your needs while maintaining the standards required for healthtech and medtech projects.

.png)
.png)
.png)

.png)




.png)
.png)




















