BitLab Teams Up with Scope Technologies and Global Care Innovations to Advance Healthcare AI
Read More

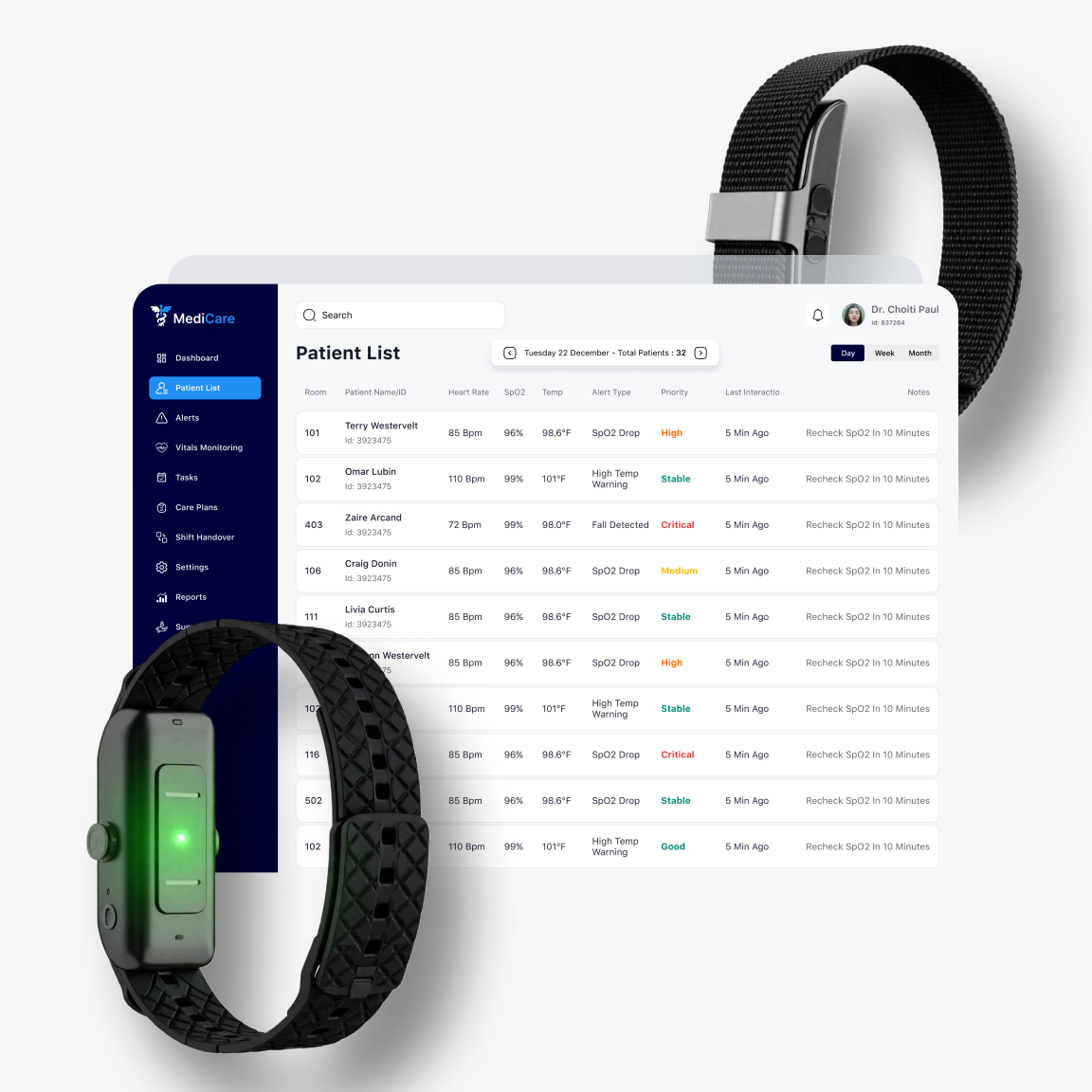
AI-powered bedside assistant triages requests, tracks pain and mood, and keeps care on course.
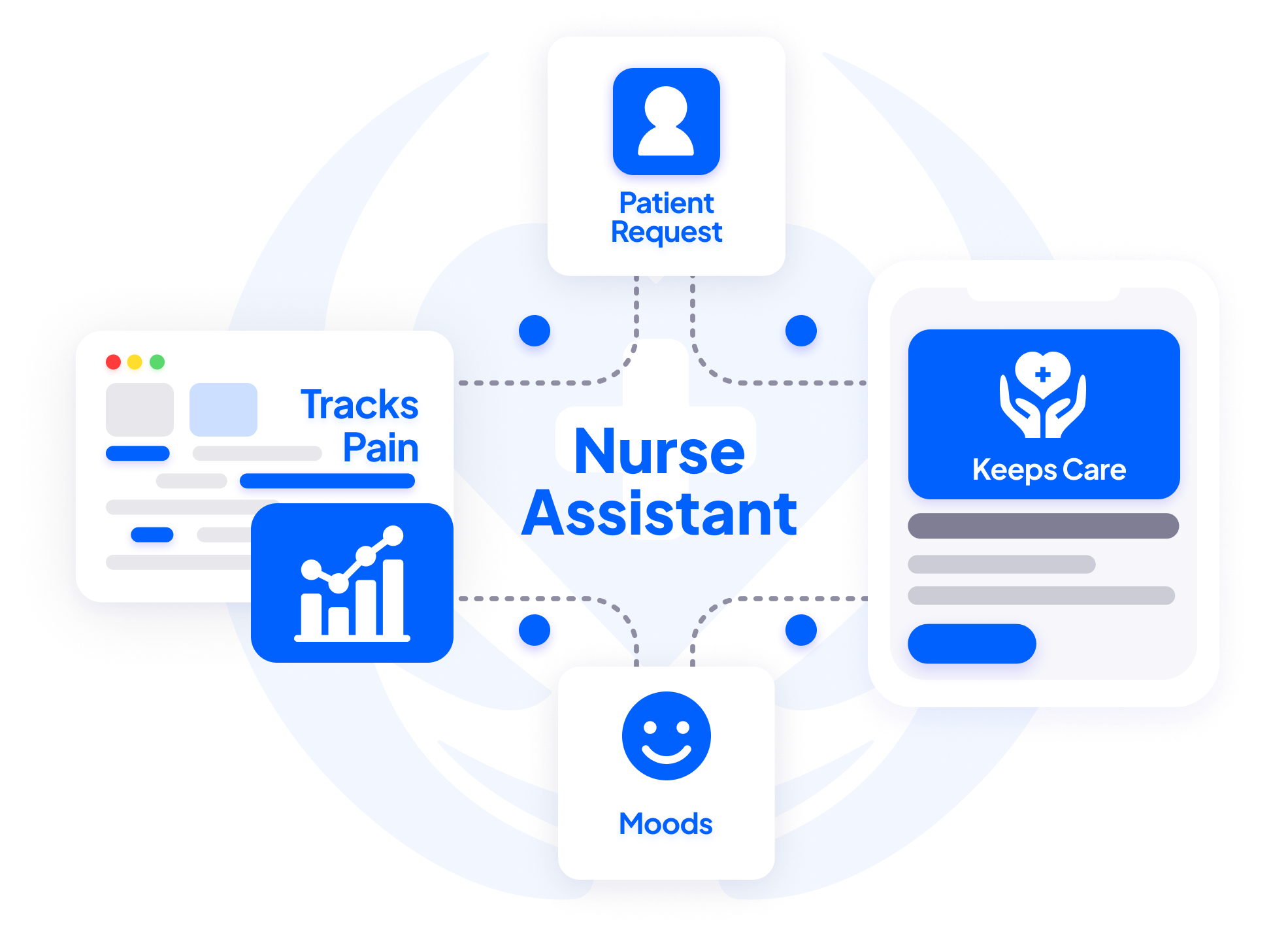
The agent collects routine requests and triages what matters.
The bedside assistant responds via touchscreen or voice input—instantly.
The AI tracks mood, pain, and soft symptoms—escalating early when needed.
The agent automates rounds for low-acuity needs, freeing up nurse bandwidth.
The assistant explains labs, meds, and care plans in simple, patient-friendly terms.
- Offload routine check-ins and education to AI
- Extend nursing presence to every room, 24/7
- Track mood, pain, and changes proactively
- Escalate deteriorations before they reach crisis level
- Handle hydration, bathroom, pain check-ins automatically
- Reduce unnecessary interruptions to clinical staff
- Clarify care instructions, medications, and discharge steps
- Reduce confusion, anxiety, and avoidable readmissions
BitLab specializes in helping medical professionals convert medical insights into compliant, investor-ready healthtech platforms.


















and 40+ others
A 76-year-old patient recovering from knee replacement became increasingly anxious and disoriented during the night. Nurses, stretched across 12 rooms, missed the early signs. By morning, the patient had experienced a fall while attempting to walk to the restroom unattended.
Mood or behavior changes were not captured because no vital signs were outside normal range. No one realized the patient was restless or confused until the fall occurred. The call bell wasn't pressed, and nurses were unaware of any issue.
- Patient sustained a minor fracture
- Length of stay extended by 2 days
- Internal review flagged failure in subjective monitoring
The AI would have:
- Prompted hourly mood and comfort check-ins via bedside tablet
- Detected increased agitation and flagged the change from baseline
- Triggered a non-urgent alert for overnight rounding staff
→ Fall prevented through early detection
→ Improved continuity of care overnight
→ Lower legal and quality-of-care risk for hospital

Oncology nurses were fielding nonstop patient calls—for blankets, water, and “just someone to talk to.” While compassionate care is core to the unit’s culture, these calls overwhelmed nursing bandwidth and delayed med passes and symptom checks.
The nurse call system lacked triage logic. Nurses treated all calls with equal urgency, burning time on non-clinical needs. Patient satisfaction dropped despite best efforts because clinical responsiveness suffered.
- 40% of nurse calls were non-urgent
- Staff burnout and higher turnover risk
- Patient pain med delivery frequently delayed
The AI would have:
- Handled low-priority requests (e.g. comfort, hydration, reassurance)
- Automatically queued non-urgent issues and kept patients engaged
- Escalated only high-priority needs (e.g. nausea, pain, bleeding)
→ Fewer interruptions for nurses
→ Faster response to clinical issues
→ Higher satisfaction without adding FTEs

New mothers were discharged with verbal instructions and a printed care packet. Several failed to follow postnatal medication guidance correctly. One patient returned to the ED with complications from a missed warning sign listed in the discharge document—but never read.
Discharge education wasn’t absorbed. Nurses were too pressed for time to deliver tailored instruction. Patients were overwhelmed and forgot what they were told.
- 2 patients readmitted for preventable issues
- CMS penalties triggered under readmission benchmarks
- Nurse dissatisfaction with rushed discharge routines
The AI would have:
- Provided bite-sized, interactive discharge education via tablet
- Repeated key instructions on meds, follow-ups, danger signs
- Logged education completion and follow-up compliance
→ Fewer avoidable readmissions
→ Clearer understanding of discharge instructions
→ Nurses spent less time repeating complex info